- CMS: Medicare Program; Implementation of Prior Authorization for Select Services for the Wasteful and Inappropriate Services Reduction (WISeR) Model
- Public Inspection: CMS: Medicare Program: Implementation of Prior Authorization for Select Services for the Wasteful and Inappropriate Services Reduction Model
- CMS: Secretarial Comments on the CBE's (Battelle Memorial Institute) 2024 Activities: Report to Congress and the Secretary of the Department of Health and Human Services
- HHS: Patient Protection and Affordable Care Act: Marketplace Integrity and Affordability
- HRSA Announces Action to Lower Out-of-Pocket Costs for Life-Saving Medications at Health Centers Nationwide
- Public Inspection: HHS: Patient Protection and Affordable Care Act: Marketplace Integrity and Affordability
- Increased Risk of Cyber Threats Against Healthcare and Public Health Sector
- Eight Hospitals Selected for First Cohort of Rural Hospital Stabilization Program
- Announcing the 2030 Census Disclosure Avoidance Research Program
- CMS: Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2026 Rates; Requirements for Quality Programs; and Other Policy Changes; Correction
- CMS: Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2026 Rates; Requirements for Quality Programs; and Other Policy Changes; Correction
- CMS: Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly; Correction
- CMS: Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly; Correction
- CMS: Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program for Federal Fiscal Year 2026
- CMS: Medicare Program; FY 2026 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Program Requirements
New Federal Rural Network Planning Grants Awarded
The Federal Office of Rural Health Policy (FORHP) is pleased to announce over $2.4M has been awarded to 25 rural community healthcare organizations in Fiscal Year 2019 for the new competitive funding cycle of the Rural Health Network Development Planning (Network Planning) Program. The Network Planning Program is a one-year grant program designed to promote the planning and development of integrated health care networks, specifically network participants who do not have a history of formal collaborative efforts in order to achieve efficiencies; expand access to, coordinate, and improve the quality of essential health care services; and strengthen the rural health care system as a whole.
States Awarded for High-Performing Rural Hospitals
. On July 11, 2019, HRSA’s Federal Office of Rural Health Policy (FORHP) recognized ten states as top performers in their work to improve the quality of care at rural hospitals. The states – Pennsylvania, Massachusetts, Michigan, Utah, Alabama, Nebraska, Illinois, Maine, Minnesota, and Wisconsin – have engaged in the FORHP-funded Medicare Beneficiary Quality Improvement Project (MBQIP), a project across 45 states designed to help federally-designated Critical Access Hospitals (CAHs) improve patient outcomes through quality reporting. Before this project, there was no federal program focused on helping these low volume hospitals prioritize quality reporting and improvement. MBQIP sets rural-specific measures for quality and provides technical assistance and resources to help CAHs improve.
Rural Community Ambulance Agency Transformation Self-Assessment and Resources Now Available!
A new emergency medical services (EMS) resource has been announced by the Technical Assistance and Services Center (TASC), a program of the National Rural Health Resource Center. This resource was supported by the Federal Office of Rural Health Policy and coordinated by TASC.
This resource helps ambulance agency leaders in rural America assess their agency’s readiness to transform to the level of care that is a people-centered and rewards positive patient outcomes through value-based payment. It provides assistance to rural ambulance agency leaders in succeeding with moving from volume to value in their agency’s culture and operations.
Rural Community Ambulance Agency Transformation consists of a self-assessment and associated resource collections in the areas of the Critical Access Hospital Blueprint for Performance Excellence, adapted specifically for rural ambulance agencies, from the Baldrige Excellence Framework for Health Care. Leaders are encouraged to complete the assessment periodically to monitor their progress and receive updated resources to guide their continued journey. The self-assessment and resource collections Include:
With Rural Health Care Stretched Thin, More Patients Turn To Telehealth
July 7, 2019, National Public Radio’s Life and Health in Rural America’s Series

After a difficult time in her life, Jill Hill knew she needed therapy. But it was hard to get the help she needed in the rural town she lives in, Grass Valley, Calif., until she found a local telehealth program.
Telehealth turned Jill Hill’s life around.
The 63-year-old lives on the edge of rural Grass Valley, an old mining town in the Sierra Nevada foothills of northern California. She was devastated after her husband Dennis passed away in the fall of 2014 after a long series of medical and financial setbacks.
“I was grief-stricken and my self-esteem was down,” Hill remembers. “I didn’t care about myself. I didn’t brush my hair. I was isolated. I just kind of locked myself in the bedroom.”
Hill says knew she needed therapy to deal with her deepening depression. But the main health center in her rural town had just two therapists. Hill was told she’d only be able to see a therapist once a month.
Then, Brandy Hartsgrove called to say Hill was eligible via MediCal (California’s version of Medicaid) for a program that could offer her 30-minute video counseling sessions twice a week. The sessions would be via a computer screen with a therapist who was hundreds of miles south, in San Diego.
Hartsgrove co-ordinates telehealth for the Chapa-de Indian Health Clinic, which is a 10-minute drive from Hills’s home. Hill would sit in a comfy chair facing a screen in a small private room, Hartsgrove explained, to see and talk with her counselor in an otherwise traditional therapy session.
Hill thought it sounded “a bit impersonal;” but was desperate for the counseling. She agreed to give it a try.

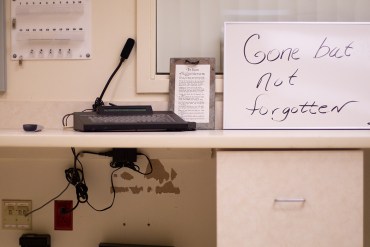
Coordinator Brandy Hartsgrove demonstrates how the telehealth connection works at The Chapa-de Indian Health Clinic in Grass Valley, Calif. Via this video screen, patients can consult doctors hundreds of miles away.
Hill is one of a growing number of Americans turning to telehealth appointments with medical providers in the wake of widespread hospital closings in remote communities, and a shortage of local primary care doctors, specialists and other providers.
Long-distance doctor-to-doctor consultations via video also fall under the “telehealth” or “telemedicine” rubric.
A recent NPR poll of rural Americans found that nearly a quarter have used some kind of telehealth service within the past few years; 14% say they received a diagnosis or treatment from a doctor or other health care professional using email, text messaging, live text chat, a mobile app, or a live video like FaceTime or Skype. And 15% say they have received a diagnosis or treatment from a doctor or other health professional over the phone.
Click here to access the entire article.
How the Federal Government Supports State and Local Efforts to Improve Rural Health: A Q&A with Tom Morris

Tom Morris, M.P.A., is associate administrator of rural health policy for the Health Resources Services Administration (HRSA), an agency of the U.S. Department of Health and Human Services (HHS). With a budget of $317 million, his office oversees a wide range of activities—from conducting research and policy analysis to providing technical assistance to hospitals in danger of closing. His office also recently assumed responsibility for administering a new program that targets the federal response to the opioid crisis to the particular needs of rural communities.
Morris took part in regional meetings of the Reforming States Group, the Milbank Memorial Fund’s bipartisan network of state executive and legislative leaders. As described in our issue brief, Supporting Rural Health: Options for State Policymakers, the meetings focused on rural health concerns and spotlighted actionable solutions.
The Milbank Memorial Fund asked Morris how HRSA and other federal agencies are working to support these approaches, including health care delivery models that promote population health, rural health workforce development, and research and policy focused on rural communities.
As a group, rural residents are older and poorer than other Americans and have worse access to health care services, as well as higher mortality rates from potentially preventable conditions. Some parts of rural America have also been ravaged by “deaths of despair” from alcohol, drug overdoses, or suicide. How is the Office of Rural Health Policy working to address these multifaceted issues?
Part of what we do is to quantify these problems so we can make sure rural issues are front and center when policy issues are considered. The opioid crisis is a good example. A lot of the initial research, both at HHS and nationally, tended to focus on opioid overdose rates at the state level. We weren’t seeing a lot about what happens in rural communities. We try to fill those gaps with research and by gathering perspectives from rural communities. Click here to read the full interview!
Rural Hospitals Support Wage Index Reform
Hospital and health system executives and practitioners were largely supportive of the CMS’ proposed changes to the wage index that they say has disproportionately impacted rural providers.
Hospital presidents and concerned employees, predominantly from rural areas, claim in some of more than 2,000 public comments that the “fundamentally flawed” system the CMS uses to set hospital payments has led to hospital closures. They hope that the agency’s plan in October to raise the index for low-wage hospitals at the expense of decreasing it for high-wage hospitals will close a wide payment disparity. Click here to access the July 3, 2019 article from Modern Healthcare.
ARC Issues County Economic Status Designations for FY 2020
The Appalachian Regional Commission (ARC) has released its County Economic Status Designations for Fiscal Year 2020, which annually ranks the economic status of each of the Region’s 420 counties using national data. According to the rankings, 80 Appalachian counties — the lowest number in over a decade — will be considered Distressed (ranking among the worst 10% of counties in the nation). Meanwhile, 110 counties will be considered At-Risk (ranking between the worst 10–25% of counties in the nation); 217 counties will be considered Transitional (ranking between worst 25% and best 25% of counties in the nation); 10 counties will be considered Competitive (ranking between best 25% and best 10% of counties in the nation); and 3 counties will be considered Attainment (ranking among the best 10% of counties in the nation). The report also shows that 29 Appalachian counties across 8 states experienced positive shifts in the economic status since FY 2019. This primarily includes counties in Alabama, Georgia, and Mississippi which each have five or more counties experiencing positive economic status shift. At the same time, 18 Appalachian counties will experience negative shifts in their economic status since FY 2019. This primarily includes coal impacted counties in Ohio, West Virginia, and Pennsylvania.
To determine the economic status of each of the Region’s 420 counties, ARC applies a composite index formula drawing on the latest data available on per capita market income combined with the previous three-year average unemployment rate, and the previous five-year poverty rates. With this data, each county is classified into one of the five economic designations. An analysis of the data also found that poverty rates in Appalachia and the nation as a whole dropped 0.4 percentage points and 0.5 percentage points respectively. This finding shows a widening gap between Appalachia’s poverty rate (16.3 percent) and the nation’s rate (14.6 percent).
The County Economic Status Designations help determine match requirements for ARC grants.
Have Cancer, Must Travel: Patients Left In Lurch After Hospital Closes
This is the first installment in Kaiser Health News’ year-long series, No Mercy, which follows how the closure of one beloved rural hospital disrupts a community’s health care, economy and equilibrium.
FORT SCOTT, Kan. — One Monday in February, 65-year-old Karen Endicott-Coyan gripped the wheel of her black 2014 Ford Taurus with both hands as she made the hour-long drive from her farm near Fort Scott to Chanute. With a rare form of multiple myeloma, she requires weekly chemotherapy injections to keep the cancer at bay.
Continuity of care is crucial for cancer patients in the midst of treatment, which often requires frequent repeated outpatient visits. So when Mercy Hospital Fort Scott, the rural hospital in Endicott-Coyan’s hometown, was slated to close its doors at the end of 2018, hospital officials had arranged for its cancer clinic — called the “Unit of Hope” — to remain open.
The full article can be accessed here.
Updates to PA Free Quitline
The Pennsylvania Department of Health’s Division of Tobacco Prevention and Control, in consultation with the National Jewish Health and Public Health Management Corporation, is implementing changes in cessation products by the PA Free Quitline. As of July 1, 2019, a 3-month supply of Chantix will be offered to newly enrolled Quitline participants on Medicaid.
HRSA Releases Updated HPSA Lists
The Health Resources and Services Administration announced the release of an updated list of geographic areas, population groups, and facilities designated as primary care, mental health, and/or dental care Health Professional Shortage Areas.
