U.S. News & World Report last week released its state health care rankings, which are based on measures of states’ access to care, health care quality, and public health. Hawaii topped the list as the best state for health care, while Mississippi ranked last. (Source: Becker’s Hospital Review.
AAMC Releases Report on Physician Shortage
The American Association of Medical Colleges (AAMC) has released the AAMC Report on Physician Shortage, its annual report on workforce shortages for health care across the nation. This year’s report projects a primary care physician shortage of 21,100 to 55,200 physicians by 2032. The shortfall range reflects the projected rapid growth in the supply of advance practice RNs and physician assistants and their role in care delivery, trends that might strengthen the nation’s primary care foundation and improve access to preventive care. The projection is based on an estimate by the Health Resources and Services Administration that nearly 14,472 primary care physicians are needed to remove the primary care shortage designation from all currently designated shortage areas. Causes of the shortfall include increasing demand from an aging population, expected retirements of many aging physicians, shorter work hours demanded by today’s physician workforce, and the growth in demand from striving to meet population health goals.
New Report Examines Financial Health of Pennsylvania Hospitals
The Pennsylvania Health Care Cost Containment Council (PHC4), the independent state agency that collects and analyzes comparative information on healthcare organizations, has released its latest report on hospitals. PHC4 Executive Director Joe Martin noted the report shows Pennsylvania general acute care hospitals’ uncompensated care again decreased, as it has in each of the past five years, to $750 million in fiscal year 2018 from $766 million the previous year. The decline can be tied to provisions in the Affordable Care Act that improve access to health insurance, particularly for those unable to get coverage at their place of employment. The independent state agency’s study also showed the statewide average operating margin for hospitals decreased to 4.76% from 5.15% during the same time period.
New Brief Comparing Characteristics of Communities served by Critical Access Hospitals

The Flex Monitoring Team has published a new brief comparing the characteristics of communities served by Critical Access Hospitals (CAHs) predicted to be at high risk of financial distress to communities served by all other CAHs. Using data from 2017, the Financial Distress Index (FDI) model assigns CAHs to high, mid-high, mid-low, or low predicted risk levels for 2019 using Medicare cost reports and Neilsen-Claritas data summed to market areas.
CAHs predicted to be at high risk of financial distress were found to serve communities with significantly higher percentages of non-White individuals (Black individuals in particular), lower high school graduation rates, higher unemployment rates, and worse health status.
Opportunities to Advance Complex Care in Rural and Frontier Areas
People with complex care needs who live in rural communities face many of the same challenges experienced by individuals in urban areas, such as lack of transportation and food insecurity. However, rural communities are not just scaled-down cities. Despite facing similar challenges to patients living in urban areas, individuals with complex needs in rural areas often face additional hurdles caused by lack of infrastructure and geographic distances, making many high-touch complex care interventions difficult — if not impossible — to implement.
This brief, made possible through the Robert Wood Johnson Foundation, explores challenges associated with providing complex care in rural and frontier communities and outlines opportunities to ensure effective programs. Drawing from experts across the country, it summarizes strategies to improve complex care delivery in rural areas and provides examples of rural communities that are enhancing care delivery through workforce adaptations, technology innovations, tailored patient engagement tactics, and new payment models and funding streams.
The brief can be accessed at https://www.chcs.org/resource/opportunities-to-advance-complex-care-in-rural-and-frontier-areas/.
Report Released on Preventive Health Service Use Among Rural Women
This study from the Maine Rural Health Research Center examined receipt of preventive health services (cholesterol check, fasting blood sugar test, mammogram, pap smear, and vaccination for the human papillomavirus, also known as HPV) by rural and urban women over the age of 18. Findings indicate that rural women were less likely than their urban peers to receive preventive health services. The report can be accessed at https://www.ruralhealthresearch.org/alerts/279.
Reports Released on Trends and Geographic Variation of Hospitals at Risk of Financial Distress
This week, the Rural Health Research Gateway released three policy briefs with the most up-to-date data on factors contributing to rural hospital closures. The producer of these briefs, the North Carolina Rural Health Research Center, keeps track of rural hospital closures and counts 104 since January 2010. The reports can be accessed at https://www.ruralhealthresearch.org/alerts/281.
USDA Releases Report on Rural Broadband and Benefits of Next Generation Precision Agriculture
Reliable, High-Speed Broadband e-Connectivity is Essential to Enhanced Agricultural Production
WASHINGTON, April 30, 2019 – Agriculture Secretary Sonny Perdue today unveiled a groundbreaking report, A Case for Rural Broadband: Insights on Rural Broadband Infrastructure and Next Generation Precision Agriculture Technologies (PDF, 2.5 MB). The report finds that deployment of both broadband e-Connectivity and Next Generation Precision Agriculture Technology on farms and ranches throughout the U.S. could result in at least $47 billion in national economic benefits every year.
“Broadband and Next Generation Precision Agriculture are critical components for creating vital access to world-class resources, tools and opportunity for America’s farmers, ranchers, foresters and producers,” Secretary Perdue said. “Under the leadership of President Trump, USDA is committed to doing our part to clear the way for nationwide broadband connectivity that will allow the next generation of precision agriculture technologies to thrive and expand.”
Download A Case for Rural Broadband: Insights on Rural Broadband Infrastructure and Next Generation Precision Agriculture Technologies (PDF, 2.5 MB). To see how Next Generation Precision Agriculture Technologies can work on farm and ranching operations, view the Connected Technologies infographic (PDF, 910 KB).
The report also finds that if broadband infrastructure and digital technologies at scale were available at a level that meets estimated producer demand, the U.S. economy could realize benefits equivalent to nearly 18 percent of total agriculture production. Of that 18 percent, more than one-third is dependent on broadband e-Connectivity, equivalent to at least $18 billion in annual economic benefits that only high-speed, reliable internet can provide.
For many years, USDA and the American agriculture industry have been actively researching the feasibility, usage and potential upside of Next Generation Precision Agriculture technologies. Until now though, the interdependency of these technologies and broadband e-Connectivity has not been evaluated. The report released today explores this symbiotic relationship and quantifies the potential economic benefit of broadband buildout and the complementary adoption of connected agriculture technologies. Going forward, the U.S. Department of Agriculture (USDA) will be engaged in multiple facets of infrastructure and technology deployment, including financing rural capital investments and supporting producers who are exploring which Next Generation Precision Agriculture Technologies are best suited to improve their operations and serve their customers.
In April 2017, President Trump established the Interagency Task Force on Agriculture and Rural Prosperity to identify legislative, regulatory and policy changes that could promote agriculture and prosperity in rural communities. In January 2018, Secretary Perdue presented the Task Force’s findings to President Trump. These findings included 31 recommendations to align the federal government with state, local and tribal governments to take advantage of opportunities that exist in rural America. The Report identified Achieving e-Connectivity in Rural America as a cornerstone recommendation. The Administration has been executing this priority call to action through the American Broadband Initiative (ABI) (PDF, 647 KB), which reflects rural broadband build-out as one of President Trump’s directives to the Federal government. A Case for Rural Broadband: Insights on Rural Broadband Infrastructure and Next Generation Precision Agriculture Technologies (PDF, 2.5 MB) opens the next chapter in the USDA’s response to this call to action.
To view the report in its entirety, please view the Report to the President of the United States from the Task Force on Agriculture and Rural Prosperity (PDF, 5.4 MB). In addition, to view the categories of the recommendations, please view the Rural Prosperity infographic (PDF, 190 KB).
Pennsylvania Oral Health Surveillance Plan Announced
The Pennsylvania Department of Health Oral Health Program is excited to announce the publication of the 2019-2024 Pennsylvania Oral Health Surveillance Plan. The Oral Health Surveillance Plan provides a consistent source of reliable and valid information for use in the monitoring of oral health status and trends of the state and for developing, implementing, and evaluating programs to improve the oral health of Pennsylvanians.
Congressional Budget Office Releases Report on Single-Payer Health Care System
Key Design Components and Considerations for Establishing a Single-Payer Health Care System
Congressional interest in substantially increasing the number of people who have health insurance has grown in recent years. Some Members of Congress have proposed establishing a single-payer health care system to achieve universal health insurance coverage. In this report, CBO describes the primary features of single-payer systems, as well as some of the key considerations for designing such a system in the United Stat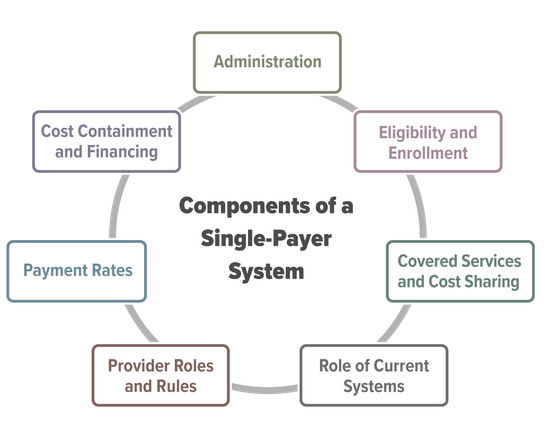 es.
es.
Establishing a single-payer system would be a major undertaking that would involve substantial changes in the sources and extent of coverage, provider payment rates, and financing methods of health care in the United States. This report does not address all of the issues that the complex task of designing, implementing, and transitioning to a single-payer system would entail, nor does it analyze the budgetary effects of any specific bill or proposal.
