- Telehealth Study Recruiting Veterans Now
- USDA Delivers Immediate Relief to Farmers, Ranchers and Rural Communities Impacted by Recent Disasters
- Submit Nominations for Partnership for Quality Measurement (PQM) Committees
- Unleashing Prosperity Through Deregulation of the Medicare Program (Executive Order 14192) - Request for Information
- Dr. Mehmet Oz Shares Vision for CMS
- CMS Refocuses on its Core Mission and Preserving the State-Federal Medicaid Partnership
- Social Factors Help Explain Worse Cardiovascular Health among Adults in Rural Vs. Urban Communities
- Reducing Barriers to Participation in Population-Based Total Cost of Care (PB-TCOC) Models and Supporting Primary and Specialty Care Transformation: Request for Input
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- 2025 Marketplace Integrity and Affordability Proposed Rule
- Rural America Faces Growing Shortage of Eye Surgeons
- NRHA Continues Partnership to Advance Rural Oral Health
- Comments Requested on Mobile Crisis Team Services: An Implementation Toolkit Draft
- Q&A: What Are the Challenges and Opportunities of Small-Town Philanthropy?
CMS: Medicare Program; FY 2021 Inpatient Psychiatric Facilities Prospective Payment System (IPF PPS)
Apr 14, 2020 — Notice of proposed rule from the Centers for Medicare and Medicaid Services updating the FY 2021 prospective payment rates, outlier threshold, and wage index for Medicare inpatient hospital services provided by inpatient psychiatric facilities (IPF), including psychiatric hospitals and excluded psychiatric units of an acute care hospital or Critical Access Hospital. The proposed rule also adopts the most recent Office of Management and Budget (OMB) statistical area delineations, and applies a 2-year transition for all providers negatively impacted by wage index changes. The changes would be effective for IPF discharges beginning October 1, 2020 – September 30, 2021. Comments on the proposed rule are due on June 9, 2020. Read more here.
CMS: Medicare Program; FY 2021 Hospice Wage Index and Payment Rate Update
Apr 15, 2020 — Notice of a proposed rule from the Centers for Medicare and Medicaid Services updating the hospice wage index, payment rates, and cap amount for fiscal year 2021. Includes changes related to the adoption of the most recent Office of Management and Budget (OMB) statistical area delineations, with a 5% cap on wage index decreases. Also summarizes the changes to the hospice election statement finalized in the FY 2020 Hospice Wage Index and Rate Update final rule and effective for October 1, 2020; and provides hospices with a model election statement and sample addendum. Includes rural considerations throughout. Comments are due by June 9, 2020. Read more here.
CMS: Medicare Program: Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Value-Based Purchasing Program for Federal Fiscal Year 2021
Apr 15, 2020 — Notice of a proposed rule from the Centers for Medicare and Medicaid Services seeking comments on updates to the prospective payment system (PPS) for skilled nursing facilities (SNFs) for fiscal year 2021. Includes proposals to make changes to the case-mix classification code mappings used under the SNF PPS, adopt the most recent Office of Management and Budget (OMB) statistical area delineations, and changes to the SNF value-based purchasing (VBP) program. Includes rural considerations throughout. Comments are due by June 9, 2020. Read more here.
FCC: Promoting Telehealth for Low-Income Consumers; COVID-19 Telehealth Program
Apr 9, 2020 — The Federal Communications Commission has released a rule to establish the COVID-19 Telehealth Program and the Connected Care Pilot Program. The COVID-19 Telehealth Program provides $200 million for healthcare providers to provide connected care services to patients in their homes or mobile locations in response to the COVID-19 pandemic. This program is effective April 9, 2020. The Connected Care Pilot Program will provide up to $100 million over three years to examine how the Universal Service Fund can support the trend toward connected care services to consumers, particularly for low-income and veteran populations. The Connected Care Pilot Program will be effective once approved by the Office of Management and Budget. Read more here.
HHS, CDC: Approval Tests and Standards for Air-Purifying Particulate Respirators
Apr 14, 2020 — Notice of interim final rule with comment period to update the regulatory requirements used by the National Institute for Occupational Safety and Health (NIOSH) to test and approve air-purifying particulate respirators for use in the ongoing COVID-19 pandemic. The rule will be effective April 14, 2020. Comments are due by August 12, 2020. Read more here.
Using Telehealth to Fight Infectious Disease
Telehealth has gained traction recently due to the opportunities in care and convenience it offers to both patients and providers. One of telehealth’s most relevant features, given the current COVID-19 crisis, is its ability to support social distancing and quarantine precautions. In a March 23, 2020 article “Using Telehealth to Fight Infectious Disease,” Athenahealth highlights a Utah-based health system’s use of telehealth to combat the dangers of inappropriate antibiotic prescribing and the challenge of managing infectious diseases in remote areas. Additional telehealth resources are available on the athenahealth’s health care technology knowledge hub webpage.
Innovative State Responses to the Opioid Crisis
Recently there has been an increase in federal funding to help mitigate the opioid crisis. This funding has allowed some health centers to create and expand partnerships with housing authorities in their communities. This brief provides creative treatment ideas to work with patients who have opioid use disorder (OUD) and struggle with homelessness and includes ways to partner with various housing services to best help your patients.
COVID-19 Resources for Non-English-Speaking People
The COVID-19 Health Literacy Project provides translations of essential information about COVID-19 in more than 35 languages. Harvard faculty has vetted all of the information in this project that was started by a medical student at Harvard. Patients with limited English proficiency are likely to be at higher risk for COVID-19 and its complications. These translational materials, along with a guidance article, Culturally and Linguistically Competent Care from ECRI, can help provide health centers with the information needed to communicate with those patients whose first language is not English and other patients with diverse cultural needs.
Contact Tracing – Guidance on this Path Out of Isolation
Contact tracing is what is now on everyone’s radar in order to help in the next step to begin to open up the country. Contact tracing is a process designed to halt the chain of transmission of an infectious pathogen–like the coronavirus–and slow community spread. When someone tests positive for an infectious disease, they become a “case.” Public health workers then reach out to the case to make sure they have what they need and that they are self-isolating. They will then figure out who they had contact with who may be at risk of infection, too. NPR recently released a guide on the basics of the process and how it might help society restart after the current wave of coronavirus cases.
US’s digital divide ‘is going to kill people’ as Covid-19 exposes inequalities
Amanda Holpuch, The Guardian
Exclusive research shows drop in connectivity is impacting rural and urban areas with populations already underserved by the medical system or racked with poverty
The Covid-19 crisis is exposing how the cracks in the US’s creaking digital infrastructure are potentially putting lives at risk, exclusive research shows.
With most of the country on lockdown and millions relying on the internet for work, healthcare, education and shopping, research by M-Lab, an open source project which monitors global internet performance, showed that internet service slowed across the country after the lockdowns.
“This is going to kill people,” said Sascha Meinrath, co-founder of M-Lab.
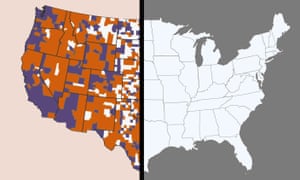
In late March, most people in 62% of counties across the US did not have the government’s minimum download speed for broadband internet, according to M-Lab.
Between February and mid March, when the pandemic was only just beginning to hit the US, there was a 10% increase in how many counties saw download speeds fall below the government standard, representing about one in 10 US counties, M-Lab found.
“Now that people’s livelihoods, schools and lives, are literally on the line, we can’t survive,” Meinrath said. “These communities that are underserved are not going to be able to transition to an online workplace or school environment.”
