- Telehealth Study Recruiting Veterans Now
- USDA Delivers Immediate Relief to Farmers, Ranchers and Rural Communities Impacted by Recent Disasters
- Submit Nominations for Partnership for Quality Measurement (PQM) Committees
- Unleashing Prosperity Through Deregulation of the Medicare Program (Executive Order 14192) - Request for Information
- Dr. Mehmet Oz Shares Vision for CMS
- CMS Refocuses on its Core Mission and Preserving the State-Federal Medicaid Partnership
- Social Factors Help Explain Worse Cardiovascular Health among Adults in Rural Vs. Urban Communities
- Reducing Barriers to Participation in Population-Based Total Cost of Care (PB-TCOC) Models and Supporting Primary and Specialty Care Transformation: Request for Input
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- 2025 Marketplace Integrity and Affordability Proposed Rule
- Rural America Faces Growing Shortage of Eye Surgeons
- NRHA Continues Partnership to Advance Rural Oral Health
- Comments Requested on Mobile Crisis Team Services: An Implementation Toolkit Draft
- Q&A: What Are the Challenges and Opportunities of Small-Town Philanthropy?
CMS Reevaluates Accelerated Payment Program and Suspends Advance Payment Program
On April 26, the Centers for Medicare & Medicaid Services (CMS) announced that it is reevaluating the amounts that will be paid under its Accelerated Payment Program and suspending its Advance Payment Program to Part B suppliers effective immediately. The agency made this announcement following the successful payment of over $100 billion to health care providers and suppliers through these programs and in light of the $175 billion recently appropriated for health care provider relief payments.
CMS had expanded these temporary loan programs to ensure providers and suppliers had the resources needed to combat the beginning stages of the 2019 Novel Coronavirus (COVID-19). Funding will continue to be available to hospitals and other health care providers on the front lines of the coronavirus response primarily from the Provider Relief Fund. The Accelerated and Advance Payment (AAP) Programs are typically used to give providers emergency funding and address cash flow issues for providers and suppliers when there is disruption in claims submission or claims processing, including during a public health emergency or Presidentially-declared disaster.
Since expanding the AAP programs on March 28, 2020, CMS approved over 21,000 applications totaling $59.6 billion in payments to Part A providers, which includes hospitals. For Part B suppliers, including doctors, non-physician practitioners and durable medical equipment suppliers, CMS approved almost 24,000 applications advancing $40.4 billion in payments. The AAP programs are not a grant, and providers and suppliers are typically required to pay back the funding within one year, or less, depending on provider or supplier type. Beginning today, CMS will not be accepting any new applications for the Advance Payment Program, and CMS will be reevaluating all pending and new applications for Accelerated Payments in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.
Significant additional funding will continue to be available to hospitals and other health care providers through other programs. Congress appropriated $100 billion in the Coronavirus Aid, Relief, and Economic Security (CARES) Act (PL 116-136) and $75 billion through the Paycheck Protection Program and Health Care Enhancement Act (PL 116-139) for health care providers. HHS is distributing this money through the Provider Relief Fund, and these payments do not need to be repaid.
The CARES Act Provider Relief Fund is being administered through HHS and has already released $30 billion to providers and is in the process of releasing an additional $20 billion, with more funding anticipated to be released soon. This funding will be used to support health care-related expenses or lost revenue attributable to the COVID-19 pandemic and to ensure uninsured Americans can get treatment for COVID-19.
For more information on the CARES Act Provider Relief Fund and how to apply, visit: hhs.gov/providerrelief.
For an updated fact sheet on the Accelerated and Advance Payment Programs, visit: https://www.cms.gov/files/document/Accelerated-and-Advanced-Payments-Fact-Sheet.pdf.
CMS COVID-19 Stakeholder Engagement Calls – Week of 4/27/20
CMS hosts varied recurring stakeholder engagement sessions to share information related to the agency’s response to COVID-19. These sessions are open to members of the healthcare community and are intended to provide updates, share best practices among peers, and offer attendees an opportunity to ask questions of CMS and other subject matter experts.
Call details are below. Conference lines are limited so we highly encourage you to join via audio webcast, either on your computer or smartphone web browser. You are welcome to share this invitation with your colleagues and professional networks. These calls are not intended for the press.
Calls recordings and transcripts are posted on the CMS podcast page at: https://www.cms.gov/Outreach-and-Education/Outreach/OpenDoorForums/PodcastAndTranscripts
CMS COVID-19 Office Hours Calls (Tuesdays and Thursdays at 5:00 – 6:00 PM Eastern)
Office Hour Calls provide an opportunity for hospitals, health systems, and providers to ask questions of agency officials regarding CMS’s temporary actions that empower local hospitals and healthcare systems to:
- Increase Hospital Capacity – CMS Hospitals Without Walls;
- Rapidly Expand the Healthcare Workforce;
- Put Patients Over Paperwork; and
- Further Promote Telehealth in Medicare
This week’s Office Hours:
Tuesday, April 28th at 5:00 – 6:00 PM Eastern
Toll Free Attendee Dial In: 833-614-0820; Access Passcode: 5787874
Audio Webcast link: https://protect2.fireeye.com/url?k=7638a38f-2a6c8aa4-763892b0-0cc47a6d17cc-cf3ef7b272885f7a&u=https://engage.vevent.com/rt/cms2/index.jsp?seid=1976
Thursday, April 30th at 5:00 – 6:00 PM Eastern
Toll Free Attendee Dial In: 833-614-0820; Access Passcode: 7476619
Audio Webcast link: https://protect2.fireeye.com/url?k=ca9c4ad8-96c94308-ca9c7be7-0cc47a6a52de-da25fff20d2e55d3&u=https://engage.vevent.com/rt/cms2/index.jsp?seid=2069
Lessons from the Front Lines: COVID-19 (Fridays at 12:30 – 2:00 PM Eastern
Lessons from the Front Lines calls are a joint effort between CMS Administrator Seema Verma, FDA Commissioner Stephen Hahn, MD, and the White House Coronavirus Task Force. Physicians and other clinicians are invited to share their experience, ideas, strategies, and insights with one another related to their COVID-19 response. There is an opportunity to ask questions of presenters.
This week’s Lessons from the Front Lines:
Friday, May 1st at 12:30 – 2:00 PM Eastern
Toll Free Attendee Dial-In: 877-251-0301; Access Code: 9545128
Weekly COVID-19 Care Site-Specific Calls
CMS hosts weekly calls for certain types of organizations to provide targeted updates on the agency’s latest COVID-19 guidance. One to two leaders in the field also share best practices with their peers. There is an opportunity to ask questions of presenters if time allows.
Home Health and Hospice (Tuesdays at 3:00 PM Eastern)
Tuesday, April 28th at 3:00 – 3:30 PM Eastern
Toll Free Attendee Dial-In: 833-614-0820; Access Passcode: 1854778 Audio Webcast Link: https://protect2.fireeye.com/url?k=946b510f-c83e58df-946b6030-0cc47a6a52de-bec23b2d515d07a0&u=https://engage.vevent.com/rt/cms2/index.jsp?seid=1856
Nursing Homes (Wednesdays at 4:30 PM Eastern)
Wednesday, April 29th at 4:30 – 5:00 PM Eastern
Toll Free Attendee Dial-In: 833-614-0820; Access Passcode: 4680237 Audio Webcast Link: https://protect2.fireeye.com/url?k=f1b73c29-ade31502-f1b70d16-0cc47a6d17cc-7bc599a5ffca4ab1&u=https://engage.vevent.com/rt/cms2/index.jsp?seid=1982
Dialysis Organizations (Wednesdays at 5:30 PM Eastern)
Wednesday, April 29th at 5:30 – 6:00 PM Eastern
Toll Free Attendee Dial-In: 833-614-0820; Access Passcode: 6965645 Audio Webcast Link: https://protect2.fireeye.com/url?k=22d566a1-7e817fdd-22d5579e-0cc47adc5fa2-3832e64127e18fa0&u=https://engage.vevent.com/rt/cms2/index.jsp?seid=2057
Nurses (Thursdays at 3:00 PM Eastern)
Thursday, April 30th at 3:00 – 3:30 PM Eastern
Toll Free Attendee Dial-In: 833-614-0820; Access Passcode: 4268398 Audio Webcast Link: https://protect2.fireeye.com/url?k=d014edc7-8c40c4ec-d014dcf8-0cc47a6d17cc-369639c42710a141&u=https://engage.vevent.com/rt/cms2/index.jsp?seid=2063
To keep up with the important work the White House Task Force is doing in response to COVID-19 click here: https://protect2.fireeye.com/url?k=36fa2226-6aae0b0d-36fa1319-0cc47a6d17cc-2d06c219f858d641&u=http://www.coronavirus.gov/. For information specific to CMS, please visit the Current Emergencies Website.
ARC Updates COVID-19 Cases in Appalachian Counties

The COVID-10 Cases in Appalachia map displays the current number of confirmed cases of COVID-19 in Appalachia and throughout the United States. Higher numbers of cases are marked by larger dots, while smaller numbers of confirmed cases are represented by smaller dots. By clicking on a location, users can see confirmed COVID-19 cases and any related deaths at the county level. This map is automatically updated throughout the day drawing on data collected by the Johns Hopkins University. Due to frequent changes, it is advised that users refresh their browsers often when viewing the map. As of April 22, there were almost 24,000 cases in 392 counties.
Congressman Jodey Arrington Pens Op-Ed on COVID-19
Congressman Jodey Arrington (R-TX-19) has written an important opinion letter in the Washington Examiner. The Texas representative calls for a flattening of the curve of rural hospital closures. The opinion letter calls on our nation’s leaders to not leave rural America without resources to combat the COVID-19 pandemic. Congressman Arrington advocated for rural access to the PPP, and for rural focused resources and funds.
New NACHC Infographic on Health Centers’ Response to COVID-19
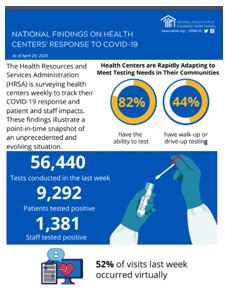 The National Association of Community Health Centers (NACHC) research team has been working with HRSA to collect data on health centers’ ongoing experiences and responses to COVID-19. The data will be updated weekly to this infographic. The infographic highlights the percentage of Federally Qualified Health Centers (FQHCs) that have the ability to test, that have walk-up or drive-up testing, the number of tests conducted by health centers in the past week, how many patients tested positive, how many employees tested positive, the percentage of visits that were conducted virtually, access to essential personal protective equipment (PPE) and challenges to health center operations.
The National Association of Community Health Centers (NACHC) research team has been working with HRSA to collect data on health centers’ ongoing experiences and responses to COVID-19. The data will be updated weekly to this infographic. The infographic highlights the percentage of Federally Qualified Health Centers (FQHCs) that have the ability to test, that have walk-up or drive-up testing, the number of tests conducted by health centers in the past week, how many patients tested positive, how many employees tested positive, the percentage of visits that were conducted virtually, access to essential personal protective equipment (PPE) and challenges to health center operations.
Has COVID-19 Changed the Course of Primary Care?
The coronavirus pandemic has hit the nation’s struggling primary care system hard. But could the crisis present an opportunity to change the way we provide and pay for primary care? A new Commonwealth Fund article highlights the shortcomings of primary care in the United States and offers strategies for building a more robust primary care system, starting with increasing what we pay primary care providers and ensuring that people can more easily get these services that are critical to maintaining health. Read more.
Battling COVID-19 Requires Testing and Contact Tracing
In an April 19 Lancaster Online op ed, Alisa Jones, CEO of Lancaster Health Center , asserts that an effective response to the COVID-19 crisis requires the public health approach of both testing and contact tracing. Citing the World Health Organization definition of contact tracing as “the systematic approach to identifying positive cases, connecting with individuals who had contact with the person who tested positive for COVID-19 and regular follow-up with those contacts to monitor for symptoms,” the article shares LCH’s experience using this approach. Ms. Jones asserts, “Widespread testing and contact tracing are how we flatten the curve of COVID-19 infection and return our community to a semblance of normalcy.” Read more.
Federal Stimulus Package 4
Congress is not expected back until May but is already discussing a fourth stimulus package to assist healthcare providers and others with the effects of the COVID-19 pandemic. NACHC is asking $73.2 billion for health centers, including $7.6 billion in emergency funding to assist with the impact of COVID-19 and $41.9 billion over five years for Health Center Program Fund reauthorization.
Pennsylvania Health Department Issues Return to Work for Healthcare Personnel Guidance
The Pennsylvania Department of Health (DOH) released PA-HAN-499 with guidance for making decisions about return to work for healthcare personnel with confirmed or suspected COVID-19. This guidance replaces PA-HAN-489. Decisions about return to work should also be made in the context of local circumstances. Options include a test-based strategy or a non-test-based strategy. If healthcare personnel must return to work before meeting criteria, they should ideally perform non-direct care or direct care for persons confirmed to have COVID-19. Click here for all the 2020 health alerts, advisories and updates.
Bipartisan Policy Center: Confronting Rural America’s Health Care Crisis
The Bipartisan Policy Center (BPC) is a think tank combining ideas and solutions from both parties. In this report, the BPC’s Rural Health Task Force makes policy recommendations to stabilize rural health care in the current emergency and the long term.

