- Submit Nominations for Partnership for Quality Measurement (PQM) Committees
- Unleashing Prosperity Through Deregulation of the Medicare Program (Executive Order 14192) - Request for Information
- Dr. Mehmet Oz Shares Vision for CMS
- CMS Refocuses on its Core Mission and Preserving the State-Federal Medicaid Partnership
- Social Factors Help Explain Worse Cardiovascular Health among Adults in Rural Vs. Urban Communities
- Reducing Barriers to Participation in Population-Based Total Cost of Care (PB-TCOC) Models and Supporting Primary and Specialty Care Transformation: Request for Input
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- 2025 Marketplace Integrity and Affordability Proposed Rule
- Rural America Faces Growing Shortage of Eye Surgeons
- NRHA Continues Partnership to Advance Rural Oral Health
- Comments Requested on Mobile Crisis Team Services: An Implementation Toolkit Draft
- Q&A: What Are the Challenges and Opportunities of Small-Town Philanthropy?
- HRSA Administrator Carole Johnson, Joined by Co-Chair of the Congressional Black Maternal Health Caucus Congresswoman Lauren Underwood, Announces New Funding, Policy Action, and Report to Mark Landmark Year of HRSA's Enhancing Maternal Health Initiative
- Biden-Harris Administration Announces $60 Million Investment for Adding Early Morning, Night, and Weekend Hours at Community Health Centers
AHA Rural Report Series: Focus on Integrated Behavioral Health Care
The American Hospital Association (AHA)’s Advancing Health Rural Report Series released a podcast in May 2019 on best practices in integrated behavioral health services.
As AHA, notes, rural hospitals are the cornerstones of their communities, serving as principal access points to care for the nearly 60 million people or 20 percent of Americans who live in rural areas. Despite their importance, rural hospitals continuously confront a multitude of challenges that threaten their ability to ensure local access to care. Hear experts talk about evidence-based programs that address behavioral health services, including Shelly Rivello, Director of Integrated Care at JC Blair Memorial Hospital, a rural hospital serving Huntingdon, PA in central Pennsylvania, who discusses the hospital’s integrated behavioral health program, The HOPE Project.
Access the podcast at https://soundcloud.com/advancinghealth/aha-rural-report-series.
Almost $1.5M Extended in Consumer Loans to Pennsylvanians with Disabilities for Assistive Technology in 2018
Harrisburg (June 3, 2019) – Pennsylvania Assistive Technology Foundation Celebrates Its Successes in 2018 and Releases its 2018-2019 Annual Report that Outlines the Organization’s Latest Accomplishments, Including the Publication of Funding Your Assistive Technology: A Guide to Funding Resources in Pennsylvania.
The latest accomplishments of Pennsylvania Assistive Technology Foundation (PATF) were highlighted at a press conference held today at the Capitol Rotunda at 10:30 a.m., hosted by Nancy Murray, President of The Arc of Greater Pittsburgh/ACHIEVA and the in-coming Board President of PATF, and Susan Tachau, Chief Executive Officer of PATF.
PATF continues to achieve outstanding results for individuals with disabilities and older Pennsylvanians, helping them purchase the assistive technology (AT) devices and services they need. The program leverages a small amount of public funding into a large number of loans that strengthen our communities. In addition, the repayment of loans from past borrowers provides funding for future borrowers. Remarkably, even though PATF makes many non-traditional loans, its loan loss rate for the last year is only 2.1%, which is better than the industry nonperformance average.
Through loans valued at more than $36M ($1.5M in 2018) and with over 14,000 Pennsylvanians helped since its founding in 1998, PATF is the only Community Development Financial Institution (CDFI) in Pennsylvania that extends consumer loans to individuals with disabilities and their families.
At today’s press conference, PATF released its 2018-2019 Annual Report, demonstrating a continued demand for its financial products. The Report highlights the following noteworthy statistics for 2018-19:
- 278 no-interest or low-interest consumer loans were extended worth $1.5M.
- More than 1,178 people were helped through Information & Assistance (I&A) services.
- 122 trainings were conducted about financial education, funding resources and assistive technology.
Nancy Murray spoke about the importance of helping people with disabilities and family members navigate the complexities of financing their AT needs. She urged everyone to pick up a copy of PATF’s new, comprehensive book, Funding Your Assistive Technology: A Guide to Funding Resources in Pennsylvania. Published in April, 454 people have already downloaded the book from PATF’s website, www.patf.us.
Susan Tachau thanked Governor Wolf and the General Assembly for their long-standing support of PATF. She stated, “We are so grateful to the Governor and our elected officials for making it possible for PATF to help Pennsylvanians with disabilities of all ages and incomes help themselves. Most of our borrowers do not have access to conventional lending markets-and therefore, do not have access to the capital that’s needed to purchase assistive technology. We remain committed to creating programs that are meaningful and respond to our ever-changing world of technology.”
Pennsylvania policymakers spoke about their continued commitment to provide essential public and private funding for the program. Speakers included:
- Senators Camera Bartolotta, Bob Mensch, and Christine Tartaglione; and
- Representatives Sheryl Delozier, Patty Kim, Brandon Markosek, and Melissa Shusterman.
Additional speakers included:
- Ms. D.J. Stemmler, PATF borrower featured in the 2018-2019 Annual Report, stated “PATF was willing to fund the van and the adaptive equipment-something most commercial banks won’t do. Without this loan, I wouldn’t have been able to continue to work.”
- David Gates, Esq., Senior Attorney, PA Health Law Project and PATF Board member, who discussed the importance of integrating financial education into community programming and he encouraged attendance at PATF’s upcoming conference, Vision for the Future: Financial Empowerment for Individuals with Disabilities on October 3, 2019 at the Keystone Building, Harrisburg.
- Matthew Seeley, Esq., Executive Director, PA Statewide Independent Living Council, who discussed blending PATF funding with PA Office of Vocational Rehabilitation (OVR) funds for the purchase of his van so that he could work and be active in the community.
- Abbie Spackman and Kendra Martin, PA AgrAbility Project, who talked about PA’s AgrAbility Program, a program that helps farmers with disabilities remain in production agriculture, and their collaboration with PATF.
Nancy Murray closed the press conference by announcing that PATF was honored to be included again in the Governor’s proposed budget for fiscal year 2020 in a line item called Assistive Technology Financing (or Devices), within the Department of Labor & Industry. The appropriation supports PATF’s operations on behalf of people with disabilities of all ages and incomes throughout the Commonwealth. PATF is advocating for an increase of $50,000 (total of $500,000) to support the costs associated with outreach and underwriting new loan applications and providing financial education trainings and one-on-one coaching.
About PATF
Pennsylvania Assistive Technology Foundation (PATF), founded in 1998, provides education and financing opportunities for people with disabilities and older Pennsylvanians, helping them to acquire assistive technology devices and services that improve the quality of their lives. It is headquartered in King of Prussia, PA and uses a network of Funding Assistance Coordinators across the state to assist prospective borrowers. The organization’s website is www.patf.us. Contact them at (888) 744-1938, or patf@patf.us. PATF is also on Facebook and Twitter.
Contact:
Susan Tachau, CEO
1-888-744-1938
National Human Trafficking Prevention Action Plan: Request for Input
The U.S. Department of Health and Human Services, Administration for Children and Families (ACF) has mobilized toward a National Human Trafficking Prevention Action Plan, which was formally announced on April 24th by Assistant Secretary Lynn Johnson during the opening session of the 21st National Conference on Child Abuse and Neglect.
“Today, we are rolling out an initiative to develop a robust national human trafficking prevention action plan. We seek partnerships with states, tribes, non-government organizations, and the private sector to amplify national and local conversations on what is working to prevent human trafficking and scale out solutions. We seek to collaborate with state and county child welfare systems and researchers to reduce vulnerabilities to trafficking. We want to identify the youth in our care who are at high risk for human trafficking so that we can intervene before another child experiences the trauma of human trafficking.” – Lynn A. Johnson, Assistant Secretary for Children and Families
Request for Information
The Office on Trafficking In Persons (OTIP) welcomes input from diverse perspectives on strengthening the Nation’s efforts to prevent human trafficking at primary, secondary, and tertiary prevention levels and that impact any level in the socio-ecological model (individual, relationship, community, and societal).
OTIP seeks information on existing programs, education, and activities to prevent the human trafficking of children and adults. OTIP aims to learn more about prevention activities pertaining to sex trafficking, labor trafficking, specialized populations, domestic victims, and foreign victims of trafficking.
The feedback received will inform a national human trafficking prevention resources clearinghouse and the development of a National Human Trafficking Prevention Action Plan.
How do I submit information?
Please send comments to EndTrafficking@acf.hhs.gov with the subject line “Human Trafficking Prevention” by July 31, 2019. Contact Alexis.Polen@acf.hhs.gov with any questions.
Additional Information
Please share with any partners that may be interested. Thanks!
New Pre-K for Pennsylvania Report Released This Week
 New Pre-K for PA Report Released This Week
New Pre-K for PA Report Released This Week
This week the Pre-K for PA Campaign released a report, Ready to Succeed: Kindergarten Teachers Support Investments in High-Quality Pre-k, based on findings of a survey conducted with campaign partner PSEA. The results show resounding support for high-quality pre-k among those surveyed.
PPC President and CEO Kari King joined fellow campaign members at an event at Hamilton Elementary School in the Carlisle Area School District in Cumberland County to release the report, noting, “Investments in high-quality pre-k have a significant return on investment for our children, schools and communities. However, the state is not investing enough to ensure access for the children who need it the most.”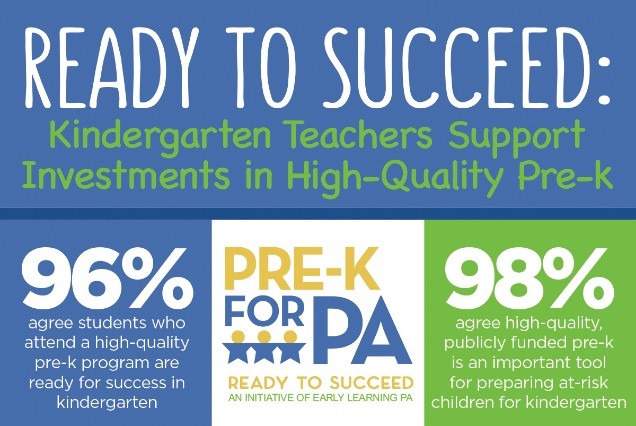
More than 97,000 – or 56 percent – of eligible 3- and 4-year-olds do not have access. The Pre-K for PA Campaign is calling for a $50 million increase in the 2019-20 state budget; $40 million for Pre-K Counts and $10 million for the Head Start Supplemental Assistance Program (HSSAP). This investment will provide access to an additional 5,500 children.
Improving Oral Health Care Services in Rural America
Improving Oral Health Care Services in Rural America. The shortage of practicing dental professionals in rural communities is influenced by a variety of factors, especially the limited number of dentists who are able and/or willing to start a rural practice. The archive of this hour-long presentation is now available, in which experts discuss policy recommendations in the recent report on this topic from the National Advisory Committee on Rural Health and Human Services.
Health Professions Training Programs Dashboard
Health Professions Training Programs Dashboard. Visit HRSA’s new dashboard at data.HRSA.gov to view data from HRSA’s Bureau of Health Workforce education and training programs for academic year 2012–2013 to present. Find out how these health workforce grant programs are supporting HRSA’s goal of providing high quality, culturally competent care in rural and underserved communities.
Supporting Rural Health: Practical Solutions for State Policymakers
Supporting Rural Health: Practical Solutions for State Policymakers. With input from HRSA’s Federal Office of Rural Health Policy, the Milbank Memorial Fund presents this issue brief with findings from three regional meetings of federal and state health officials and health services researchers working on rural issues. Case studies summarized in the brief shed light on successful models for incentivizing investment, the need for workforce development, and the need for ongoing research and policy development specifically directed toward rural health.

David B. Nash, MD, MBA, Founding Dean, Jefferson College of Population Health, has announced that the application process is now open for the 2020 Hearst Health Prize! The winner will receive a $100,000 prize in recognition of outstanding achievement in managing or improving population health. Up to two finalists will receive a cash award of $25,000 each.
The Hearst Health Prize, in partnership with the Jefferson College of Population Health (JCPH), was created to help identify and promote promising initiatives in the field that improve health outcomes. The goal is to discover, support, and showcase the work of an individual, group, or institution that has successfully implemented a population health program that has made a measurable difference.
Last year, they received over 150 impressive submissions from across the country showcasing a range of projects aimed at improving the health of populations. The 2019 winner, Sharp Transitions, was recognized at the Population Health Colloquium for its outstanding home-based palliative care program for patients with advanced and progressive chronic illness who are not ready for hospice care. Additionally, two finalists, Arkansas SAVES, and Mental health Outreach for MotherS (MOMS) Partnership® were each awarded $25,000 for their impactful programs.
Finalists will be invited to present their project during a special poster session at the Population Health Colloquium in Philadelphia, March 30-April 1, 2020. The winner of the prize will be announced during the opening session of the Population Health Colloquium on March 31, 2020.
To apply or learn more about the Hearst Health Prize visit: Jefferson.edu/HearstHealthPrize. The deadline to submit an application is Friday, August 9, 2019, 3:00 PM (EDT)/12:00 Noon PM (PDT).
If you have any questions, please email HearstHealthPrize@Jefferson.edu. Please share this amazing opportunity with your colleagues!
Medicare Dental Benefit Act Introduced in House
Representative Nanette Diaz Barragan (D-CA) introduced the Medicare Dental Benefit Act of 2019, H.R. 2951 which, if passed, will add dental coverage to Part B of the Medicare program. The legislation has now been introduced in both chambers of Congress. This is another milestone in efforts to elevate the need for improved oral health coverage in public health care programs.
Briefs Published on Identifying High-Need Rural Counties to Help in Resource Location Planning
The Rural Minority and Minority Health Research Center at the University of South Carolina has published two policy briefs.
The first brief, Identification of High-Need Rural Counties to Assist in Resource Location Planning, categorizes high-need, low-resource locations by identifying counties that lacked safety-net providers.
The second brief, Identification of High-Need Rural Counties to Assist in Resource Location Planning for Primary Care, examines areas with poor health outcomes and limited access to primary care safety net settings.
