- The Biden-Harris Administration Supports Rural Health Care
- Biden-Harris Administration Announces $52 Million Investment for Health Centers to Provide Care for People Reentering the Community after Incarceration
- On National Rural Health Day, Reps. Sewell and Miller Introduce Bipartisan Legislation to Support Rural Hospitals
- Terri Sewell Cosponsors Bill Reauthoring Program to Support Rural Hospitals
- HRSA: Inclusion of Terrain Factors in the Definition of Rural Area for Federal Office of Rural Health Policy Grants
- Celebrating National Rural Health Day
- DEA, HHS: Third Temporary Extension of COVID-19 Telemedicine Flexibilities for Prescription of Controlled Medications
- Talking Rural Health Care with U of M
- Public Inspection: DEA, HHS: Third Temporary Extension of COVID-19 Telemedicine Flexibilities for Prescription of Controlled Medications
- CDC Presents a Five-Year Plan for Rural Healthcare
- Kansas Faith Leaders 'Well Positioned' To Help Fill Mental Health Care Gaps in Rural Areas
- The CDC Wants More Kansas Farm Workers to Get Their Flu Shots This Season
- Study: Rural Residents More Likely to Struggle With Medical Debt
- Deaths From Cardiovascular Disease Increased Among Younger U.S Adults in Rural Areas
- VA Proposes to Eliminate Copays for Telehealth, Expand Access to Telehealth for Rural Veterans
How to Treat Dental Patients Who Use Marijuana
An article in Dr. BiCuspid shares information from a recent presenter at the Chicago Dental Society’s midwinter meeting who presented on how to treat dental patients who use marijuana. Smoking or ingesting marijuana can wreak havoc on the oral cavity, exacerbating gum disease and causing dry mouth, and can be life-threatening when mixed with some anesthetics. Read more.
The 2022 Medication Adherence Practice Module from Quality Insights is Released
Quality Insights has released its 2022 Medication Adherence Practice Module. This newly updated resource is designed to assist in promoting and improving your quality improvement efforts, specifically related to medication management and adherence across patient populations living with high blood pressure, hypercholesterolemia, prediabetes, and diabetes. Updates include Medication Adherence Office Protocol, enhanced care team and patient communication resources, and tips for assessing health literacy, cultural competency, and potential language barriers. Download the 2022 Medication Adherence Practice Module and Workflow Modification Guide as well as a brief module overview recording.
Pennsylvania Adds a New Health Information Organization
Pennsylvania’s health information exchange network now has a new health information organization (HIO). The Lehigh Valley Health Network has successfully completed the requirements for certification as a Pennsylvania eHealth Partnership Uniform Participant in the Pennsylvania Patient and Provider Network, or P3N. Read more.
Duquesne University in Pittsburgh Breaks Ground for Osteopathic Medical School
 Duquesne University in Pittsburgh broke ground for the new Duquesne College of Osteopathic Medicine (DCOM) on March 1. Among the speakers was Jerome Gloster, MD, CEO of FQHC Primary Care Health Services (PCHS). Dr. Gloster spoke about how PCHS has experienced Duquesne’s dedication to serving the community through their partnership with the university’s Duquesne Center for Integrated Health asthma program for children and teenagers. PCHS, East Liberty Family Health Care Center, and North Side Christian Health Center are among the healthcare organizations that will partner with DCOM to provide rotations for third- and fourth-year medical students. John Kauffman, DO, the founding dean of DCOM, said an emphasis will be placed on serving underserved communities. He anticipates that 50% of each class of residents will go into primary care. The $151 million projects is projected to take two years with the first class of students starting in 2024.
Duquesne University in Pittsburgh broke ground for the new Duquesne College of Osteopathic Medicine (DCOM) on March 1. Among the speakers was Jerome Gloster, MD, CEO of FQHC Primary Care Health Services (PCHS). Dr. Gloster spoke about how PCHS has experienced Duquesne’s dedication to serving the community through their partnership with the university’s Duquesne Center for Integrated Health asthma program for children and teenagers. PCHS, East Liberty Family Health Care Center, and North Side Christian Health Center are among the healthcare organizations that will partner with DCOM to provide rotations for third- and fourth-year medical students. John Kauffman, DO, the founding dean of DCOM, said an emphasis will be placed on serving underserved communities. He anticipates that 50% of each class of residents will go into primary care. The $151 million projects is projected to take two years with the first class of students starting in 2024.
Health Care Headlines, Business News & Trends
CDC Updates COVID-19 Masking and Monitoring Guidance
The Centers for Disease Control and Prevention (CDC) recently updated its framework to monitor the level of COVID-19 in communities. CDC leaders also announced that this data will inform recommendations on prevention measures like masking. They have updated their masks webpage to provide guidance based on the COVID-19 Community Level and personal risk factors. Read the full media briefing transcript.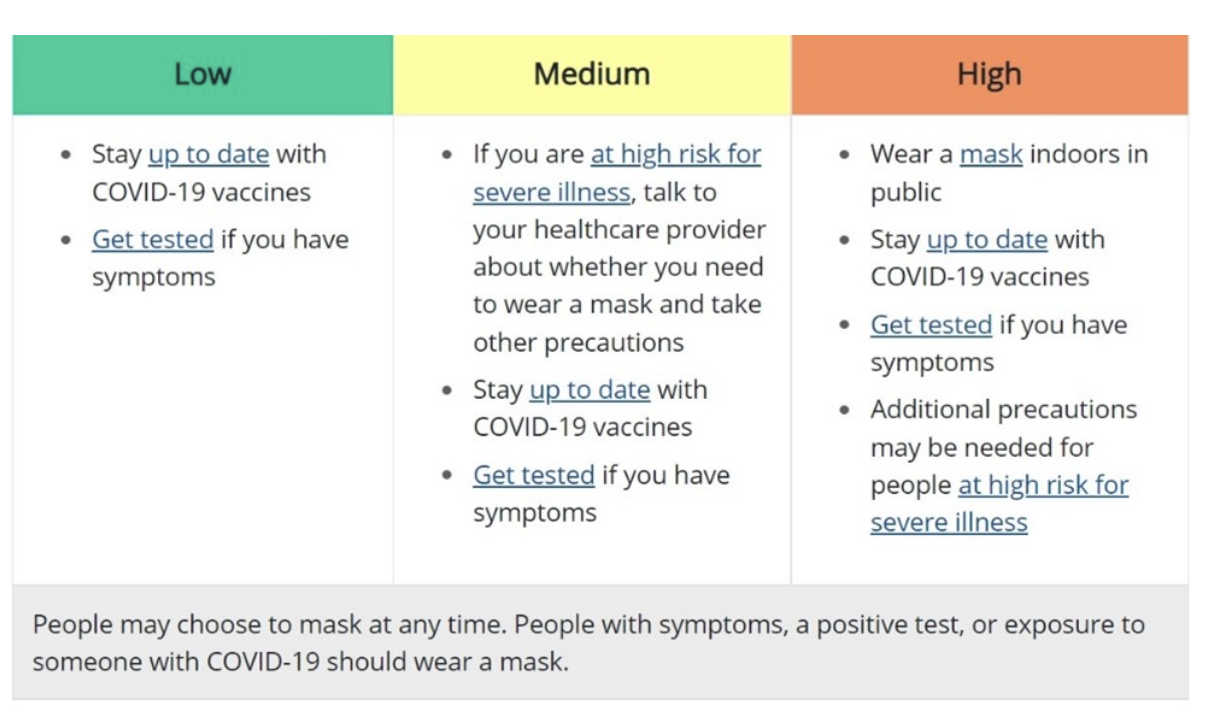
Race and Ethnicity Matter in Accessing Medical Care
The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released an issue brief on Experiences in Accessing Medical Care by Race and Ethnicity. The brief uses data from the 2015-2018 National Health Interview Survey (NHIS) to assess Medicaid members’ access to care by race and ethnicity. Notably, the study found that Black, Hispanic, and Asian Medicaid members had significantly lower rates of receiving some preventive health screenings as compared to white non-Hispanic members and that Black and Hispanic Medicaid members were less likely than white non-Hispanic members to receive primary care and mental health care visits.
$88 Billion in Medical Debt on Consumer Credit Reports
Consumer credit reports contained $88 billion in medical debt as of June, a problem the federal agency that enforces financial protection rules vows to crack down on. Medical debt is far and away from the most common type of liability on credit reports. On Tuesday, Consumer Financial Protection Bureau (CFPB) officials questioned whether it belongs there at all. As of last year, 58% of all third-party debt collections were for medical debt, the agency determined in a new report. The CFPB found that about 20% of U.S. households owe a medical debt, which appears on 43 million credit reports.
Congress Turns Their Attention to Behavioral Health
In February, Senate and House Committees held a number of hearings on behavioral health, including two Senate Finance Committee hearings on youth mental health, a Senate HELP Committee hearing on mental health and substance use, a House Energy and Commerce Committee hearing on mental health, and two House Ways and Means Committee hearings on the mental health crisis, substance use, and suicide. Senate Finance Chair Wyden (D-OR) reportedly hopes to introduce a broad bipartisan package this summer focused on the integration of primary and mental health care, telehealth, parity, and children’s behavioral health.
Pennsylvania Governor Adds New Qualifying Life Event for Pennie Coverage
Gov. Tom Wolf this week announced that Pennsylvania’s state-based health insurance marketplace, Pennie, has added a new qualifying life event to allow low-income Pennsylvanians the ability to enroll in health insurance throughout the year. This new qualifying life event will allow Pennsylvanians with an annual household income equal to or below 150% of the federal poverty level to shop and enroll in health insurance through Pennie. Financial assistance, which nearly 90% of the almost 375,000 Pennie customers receive, is also available. Pennsylvanians enrolling during 2022 can also benefit from the increased subsidies provided by the American Rescue Plan, which has changed the affordability of health coverage across the nation.
To receive this new qualifying life event through Pennie, new customers will need to visit pennie.com, click “Get Covered” and apply. If the customer meets the income qualifications, a Special Enrollment Period will automatically open. Once the Special Enrollment Period opens, the customer will have 60-days to shop and enroll in a healthcare plan through Pennie. Currently, this opportunity is only available for those currently not receiving health coverage through Pennie. Beginning June 2022, existing Pennie customers whose income is lower than or equal to the 150% federal poverty level can update their application and change their current plan using this qualifying life event.
The Department of Veteran Affairs Creates a Graduate Medical Education & Residency Pilot Program

If finalized, a proposed rule from the U.S. Department of Veterans Affairs (VA) would place medical residents in existing or new residency programs and reimburse certain costs associated with graduate medical education. The VA is considering factors for determining clinical needs in certain areas, i.e., the ratio of veterans to VA providers, and for placement of residents in facilities outside of the VA. This will include an evaluation of the range of clinical specialties of VA and non-VA providers in underserved rural and tribal communities. A future request for proposal will announce opportunities for placement of residents at certain underserved VA facilities as well as certain Rural Health Clinics and Federally Qualified Health Centers. By statute, the pilot program prioritizes the placement of residents in Indian Health Service facilities, and Indian tribal or tribal organization facilities.

