- Dr. Mehmet Oz Shares Vision for CMS
- CMS Refocuses on its Core Mission and Preserving the State-Federal Medicaid Partnership
- Social Factors Help Explain Worse Cardiovascular Health among Adults in Rural Vs. Urban Communities
- Reducing Barriers to Participation in Population-Based Total Cost of Care (PB-TCOC) Models and Supporting Primary and Specialty Care Transformation: Request for Input
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- 2025 Marketplace Integrity and Affordability Proposed Rule
- Rural America Faces Growing Shortage of Eye Surgeons
- NRHA Continues Partnership to Advance Rural Oral Health
- Comments Requested on Mobile Crisis Team Services: An Implementation Toolkit Draft
- Q&A: What Are the Challenges and Opportunities of Small-Town Philanthropy?
- HRSA Administrator Carole Johnson, Joined by Co-Chair of the Congressional Black Maternal Health Caucus Congresswoman Lauren Underwood, Announces New Funding, Policy Action, and Report to Mark Landmark Year of HRSA's Enhancing Maternal Health Initiative
- Biden-Harris Administration Announces $60 Million Investment for Adding Early Morning, Night, and Weekend Hours at Community Health Centers
- Volunteer Opportunity for HUD's Office of Housing Counseling Tribe and TDHE Certification Exam
- Who Needs Dry January More: Rural or Urban Drinkers?
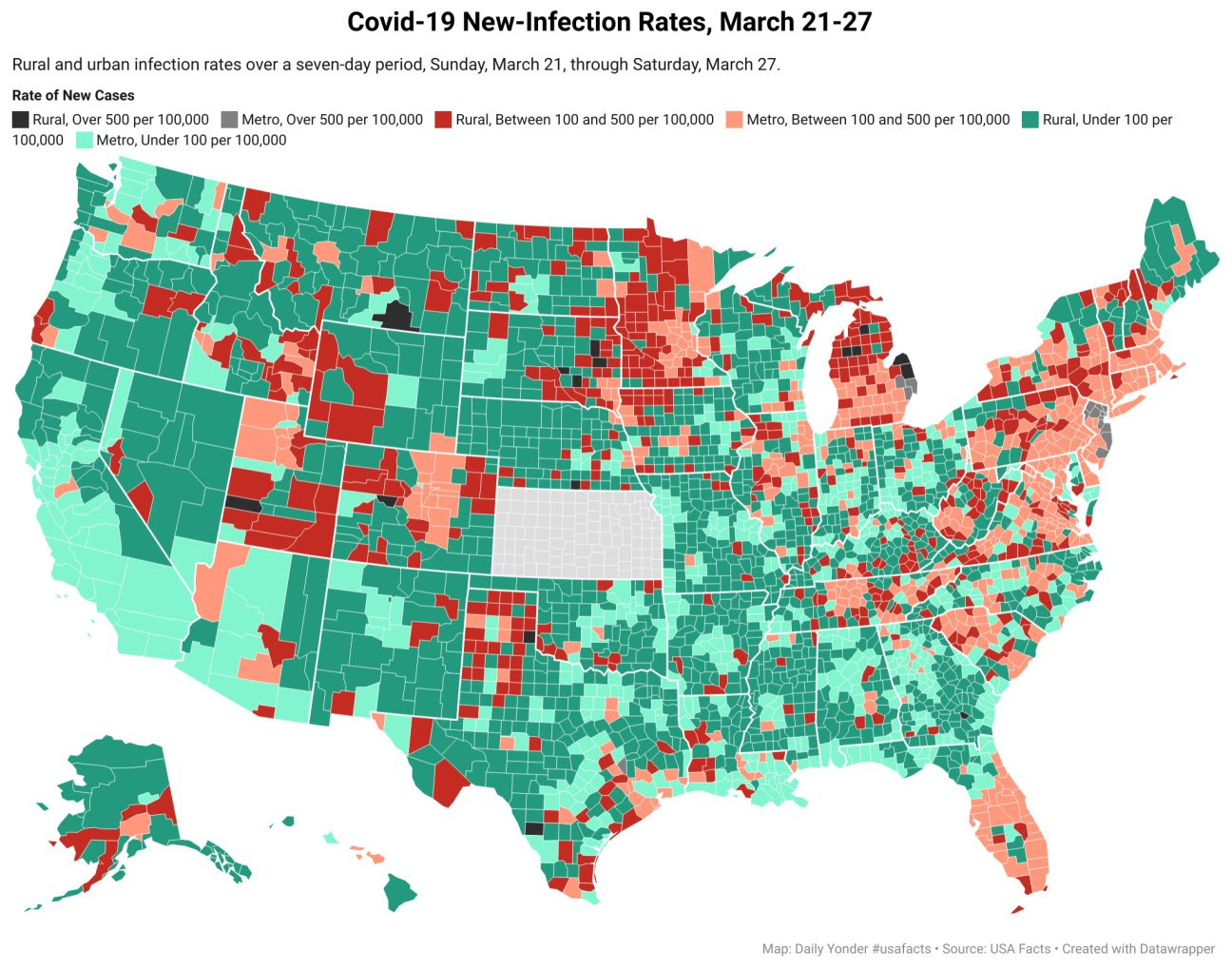
Rural Covid Cases Remain Steady but the Number of Red-Zone Counties Increases

By Tim Murphy and Tim Marema
The number of new cases in rural counties increased marginally last week, but new metropolitan cases climbed by 15%.
Read more
Research: Big-City Approaches to Legal Aid Don’t Work in Rural Settings

By Olivia Weeks
Low-income rural Americans aren’t getting equal access to justice because too many legal-aid programs are designed as if they are serving big cities, a new study says.
Read more
Rural Availability of Sexual Assault Nurse Examiners
For victims of sexual assault, high-quality health care provided by sexual assault nurse examiners (SANEs) is associated with improved health and prosecutorial outcomes. However, very little is known about access to SANEs.
Sheridan Miyamoto, assistant professor and SAFE-T Center principal investigator, and Elizabeth Thiede, nursing doctoral student and 2021 ENRS Student Conference Scholarship Award winner, wanted to learn more about whether rural areas in particular may have disparate access to SANEs.
“If rural areas have limited SANE availability, then rural victims of sexual assault may be at risk of receiving lower-quality care, which has implications not only for their health but also for prosecutorial outcomes,” stated Thiede.
The research recently was published in The Journal of Rural Health.
To examine rural access to SANEs, Thiede and Miyamoto analyzed data from the International Association of Forensic Nurses (IAFN) as well as data collected from 43 rural Pennsylvania hospitals.
The IAFN data showed that certified SANEs — those who have met rigorous qualifications and passed a certification exam — were only present in 16.7% of rural counties. The data collected from individual hospitals confirmed that very few have certified SANEs on staff and, instead, most rely on registered nurses with varying levels of additional training in sexual assault care.
Thiede and Miyamoto also found that most of these hospitals are not able to provide continuous sexual assault care coverage. This may lead them to encourage victims to seek care elsewhere or to rely on health care providers without additional training and experience in sexual assault care when victims present to emergency rooms.
Miyamoto and Thiede suspect that the absence of certified SANEs in the majority of rural Pennsylvania counties could be indicative of barriers to meeting certification requirements for rural SANEs. The two suggested one likely barrier to certification is the difficulty obtaining the supervised practice hours required for certification eligibility.
“Rural communities face challenges in recruiting, training, and retaining SANE nurses. Creative solutions are needed to increase access to quality sexual assault care.” Miyamoto stated. “The intent of the Penn State Sexual Assault Forensic Examination Telehealth (SAFE-T) program is to pair less experienced nurses working in rural areas with expert SANEs to receive examination support, precepting, and peer review via telehealth technology. Programs like this show great promise in growing and sustaining a rural SANE workforce.”
To continue ensuring that rural sexual assault victims receive expert quality sexual assault care, further research is needed to better understand how hospitals make decisions related to how they will provide sexual assault care and how ecological factors, such as hospital resources, the population size of the surrounding community, organizational culture, and state-level oversight may influence this decision-making.
More information about the SAFE-T Center and their work can be found on the website.
COMING SOON: Emergency Broadband Benefit Program
Health care centers, grantees and partners have an exciting opportunity to help spread the word about an upcoming program. Eligible patients and households may apply for the Federal Communications Commission (FCC) Emergency Broadband Benefit (EBB) program when it opens in late April.
Background
The Federal Communications Commission’s (FCC) Emergency Broadband Benefit (EBB) program lowers the cost of high-speed internet service to ensure people have the connectivity they need during the ongoing COVID-19 public health emergency. By the end of April, $3.2 billion in funding will be available to provide qualifying households discounts on their internet service bills and an opportunity to receive a discount on a computer or tablet. The EBB program is similar to the Lifeline program with expanded eligibility, vendors, and subsidies. This benefit is available directly to consumers on a first come, first serve basis.
Eligible patients and households may submit applications beginning around late April. Health centers and organizations are encouraged to begin preparing to increase awareness and help patients apply (e.g., outreach, internet access, and supporting applications completion). Organizations are encouraged to develop a plan now to support patients as funds are expected to go quickly.
How You Can Help
- Share information about the EBB program with patients.
- FCC’s EBB webpage
- Fact sheet
- Provide access to the internet and basic technical support at your organization so patients can complete the application.
The Telehealth Resource Centers are available to assist with questions. For more information, including recorded technical assistance webinars, please visit the FCC-supported technical assistance provider Universal Service Administrative Company and visit the resources below.
Resources for the EBB Program:
- FCC’s EBB webpage
- Consumer FAQ for Emergency Broadband Benefit
- Fact sheet
- “Become an Outreach Partner”
- Universal Service Administrative Company Technical Assistance Webinars
USDA Seeks Applications to Support Technical Assistance and Improve RuralTransportation Systems

U.S. Department of Agriculture (USDA) Deputy Under Secretary for Rural Development Justin Maxson announced that USDA is accepting applications for grants to improve rural transportation systems.
USDA is making the grants available under the Rural Business Development Grant program. Eligible applicants are organizations seeking to provide rural communities with training and technical assistance to improve transportation services and facilities. USDA does not provide funding directly to individuals under this program.
Applications will be scored, reviewed, and selected on a competitive basis. Applications must be submitted to the applicant’s nearest USDA office by June 30, 2021, at 4:30 p.m. local time. Additional information is available on page 17112 of the April1, 2021, Federal Register.
In Pennsylvania, please contact the Business and Cooperatives Program Director David Foster at 717-237-2181 or David.Foster@usda.gov with any questions about the program or application process.
Applicants are encouraged to consider projects that provide measurable results in helping rural communities build robust and sustainable economies through strategic investments in infrastructure, partnerships, and innovation.
USDA Seeks Public Input to Help Create a New Rural Renewable Energy Pilot Program
Agency to Host Public Listening Session on April 22
The U.S. Department of Agriculture (USDA) announced it is requesting public input from interested parties, including potential customers and interested stakeholders, to help create a new Rural Renewable Energy Pilot Program. To ensure a diverse group of voices are heard, USDA is seeking written comments and will host a public listening session on April 22, 2021.
“When we invest in creating new sources of renewable energy, we invest in rebuilding the middle class by creating good-paying jobs in rural America,” USDA Deputy Under Secretary for Rural Development Justin Maxson said. “To meet this goal, we must put rural communities at the heart of climate action and climate-smart solutions, and that begins with getting feedback from a broad, diverse set of voices from the start.”
The Consolidated Appropriations Act, 2021 (PL116-260) provided $10 million to USDA to develop a pilot program that provides financial assistance to rural communities to further develop renewable energy. This request for information and the stakeholder listening session seek input to help develop options for the Rural Renewable Energy Pilot Program. The new program will aim to support the Nation’s critical energy needs, and combat climate change while advancing environmental justice, racial equity, and economic opportunity through the use of distributed energy technologies, innovations, and/or solutions.
The stakeholder listening session will be held virtually on Thursday, April 22, 2021, 2 p.m. – 4:30 p.m. EDT. Anyone can RSVP to participate online.
Public comment is requested on the following topics:
- Program purposes, goals, metrics, and standards;
- Eligible applicants, participants, partners including but not limited to communities, residencies, industry, and commercial entities;
- Eligible technologies including but not limited to generation, storage, controller, and grid;
- Potential impact of the pilot program and renewable energy systems more broadly on each of the following: environmental justice, racial equity, and economic opportunity; and
- Options to measure and maximize the benefits of renewable energy systems for environmental justice, racial equity, and economic opportunity in rural areas.
Written comments are encouraged and must be submitted online by April 29, 2021, via the Federal eRulemaking Portal. To submit a comment, visit http://www.regulations.gov and search for the Docket ID RBS–21–Business–0010. Follow the online instructions for submitting comments. All comments received will be posted without change and will be publicly available on regulations.gov.
For additional information on the request for information and listening session, see page 16575 of the March 30, 2021, Federal Register.
Under the Biden-Harris Administration, Rural Development provides loans and grants to help expand economic opportunities, create jobs and improve the quality of life for millions of Americans in rural areas. This assistance supports infrastructure improvements; business development; housing; community facilities such as schools, public safety and health care; and high-speed internet access in rural, Tribal and high-poverty areas. For more information, visit www.rd.usda.gov. If you’d like to subscribe to USDA Rural Development updates, visit our GovDelivery subscriber page.
USDA touches the lives of all Americans each day in so many positive ways. In the Biden-Harris Administration, USDA is transforming America’s food system with a greater focus on more resilient local and regional food production, ensuring access to healthy and nutritious food in all communities, building new markets and streams of income for farmers and producers using climate, smart food and forestry practices, making historic investments in infrastructure and clean energy capabilities in rural America, and committing to equity across the Department by removing systemic barriers and building a workforce more representative of America. To learn more, visit www.usda.gov.
HHS Announces Reduced Costs and Expanded Access Available for Marketplace Health Coverage Under the American Rescue Plan

U.S. Department of Health and Human Services (HHS) Secretary Xavier Becerra announced that additional savings and lower health care costs are available for consumers on HealthCare.gov. The American Rescue Plan (ARP) has increased tax credits available to consumers, helping to reduce premiums and giving consumers access to affordable health care coverage. The Department also announced an additional $50 million in advertising to bolster the Special Enrollment Period outreach campaign. The campaign will run through August 15, 2021.
“We’re delivering lower health care costs to more Americans because everyone deserves access to quality, affordable health care. Today help is here and millions of Americans can start saving money on their health insurance premiums thanks to the American Rescue Plan,” said HHS Secretary Xavier Becerra. “The Biden Administration is committed to bringing down health care costs for families. Consumers can save money by visiting HealthCare.gov and choosing a plan that works for them and their budget. HHS will be reaching out to encourage Americans to use the Special Enrollment Period to sign up for quality, affordable coverage through HealthCare.gov.”
To read the HHS press release (English), visit: https://www.hhs.gov/about/news/2021/04/01/hhs-secretary-becerra-announces-reduced-costs-and-expanded-access-available-marketplace-health-coverage-under-american-rescue-plan.html
To read the HHS press release (Spanish), visit: https://www.hhs.gov/about/news/2021/04/01/secretario-de-salud-y-servicios-humanos-xavier-becerra-anuncia-reduccion-de-costos-y-expansion-de-acceso-a-cobertura-de-salud-en-el-mercado-de-salud-bajo-american-rescue-plan.html
To read the ASPE brief, visit: https://aspe.hhs.gov/pdf-report/access-to-low-premiums-issue-brief-part-II
‘It Didn’t Really Stick With Me’: Understanding the Rural Shrug Over COVID and Vaccines

At 70, Linda Findley has long been active in her small town of Fort Scott, Kansas, which sits more than an hour away from any major city.
Findley, whose husband died in an accident just after the local hospital closed, helps with the Elks and fundraising, and — like many people in this part of the country — doesn’t think covid-19 is that dangerous.
“I don’t even know what I think about it,” Findley said recently. “I don’t know if I trust the testing because it’s so messed up or … I’ve had nieces and nephews, that’ve had it. I’ve lost good friends to it, or supposedly it’s to that.”
Findley said she just isn’t sure that every case reported as the coronavirus really is the virus: “Everything seems to be coronavirus. I mean, it’s just … no matter what somebody has, it’s coronavirus. I don’t know whether it is or isn’t.”
Fort Scott is one of nearly 140 rural communities that have lost a hospital in the past decade. Mercy Hospital Fort Scott closed in December 2018.
Even though critically ill patients now must travel to hospitals farther away, Fort Scott residents haven’t seen that as a pandemic-related problem. Rather, not having a hospital doesn’t really come up when people here talk about COVID.
Dave Martin, the former city manager, is pretty sure he caught COVID at work last August.
“You know, when I got it, I was in good health and it did take me a while to recover,” Martin said. “I do remember waking up one of my bad nights and thinking, when I was running a temperature and not feeling very well. And I’m thinking, ‘Oh, wow, this could kill me.’”
But Martin also thought that any number of unpredictable events could end a person’s life. “So it didn’t really stick with me,” he said.
After recovering, the 62-year-old Martin went ahead with his retirement. He took his wife to Disney World and then they hiked Yellowstone National Park.
That casual attitude toward the dangers of COVID worries health care leaders in Fort Scott. Jason Wesco helps lead the regional health center that took over primary care services when the hospital closed. One clinic occupies part of the same building that used to be Mercy Hospital.
Wesco said his family is careful about wearing masks and not gathering in groups, and he believes they are in the minority in the area.
“I think most people just keep going. They have maybe modified a little bit. Maybe they put on a mask in public,” Wesco said. “I think life here has changed a lot less than it’s changed in D.C. And I think we’re seeing the impact of that, right?”
The pandemic hit the area hard in the fall, peaking in late December.
One in 11 people in Bourbon County, where Fort Scott is the largest community, has been infected by COVID, according to national analysis.
Two dozen of the county’s 14,000 residents have died of COVID. And most people know someone who had the virus and survived — but residents just seem tired of talking about it.
Community volunteer Findley said she won’t get a vaccine.
“How did they come up with a vaccine that quickly? And how do they even know for sure it’s even working?” Findley wondered.
The three vaccines approved by federal regulators in the U.S. are being given out to millions, and their efficacy has been shown through massive clinical trials in the U.S. and globally.
But Findley’s skepticism is fairly common in southeastern Kansas and across rural America. Nationwide, a smaller share of rural residents say they will definitely get a COVID shot compared with their more urban counterparts. More than a third, 35%, of those who live outside big-city borders said they would probably not or definitely not get vaccinated, compared with about a quarter of suburban and urban residents, according to a poll by KFF. (KHN is an editorially independent program of the foundation.) An NPR/PBS NewsHour/Marist Poll found that 47% of Trump supporters said they would not get a vaccine; 75% of Bourbon County residents voted for Trump in 2020.
Factors such as age and occupation also play a role in attitudes toward the vaccines. And — as Findley and others in Fort Scott noted — rural Americans are more likely to think of getting a vaccine as a personal choice and believe the seriousness of COVID is exaggerated in the news.
When Mercy Hospital Fort Scott shut its doors, locals lost care. Health workers lost jobs. The hole left behind is bigger than a hospital. Season One is “No Mercy.”
Findley said she believes that there is a very bad virus, but also that the media have brainwashed people. The news has “everybody running scared,” she said. “I don’t know why they want to do that, but that’s what I feel like.”
About 50% of rural residents say the seriousness of the coronavirus is generally exaggerated in the news, according to the KFF poll. And 62% see getting the vaccine as a personal choice — rather than a necessary social obligation.
Wesco, executive vice president of the Community Health Center of Southeast Kansas, said he has hope more area residents will begin to see the vaccines as necessary.
“There’s hesitancy,” Wesco said, adding that he believes hesitancy is declining as vaccines become more abundant.
When residents are directly provided the opportunity to get a vaccine, they consider it more seriously, he said. And the more people they know who have gotten a vaccine, the more likely they will be to get a shot.
The Community Health Center, like other health centers nationwide, is receiving direct federal shipments of vaccines. Currently, the clinic has a waitlist and is giving out as many doses as it can get its hands on.
Sarah Jane Tribble is reporter and host of “Where It Hurts,” a narrative podcast created by KHN and St. Louis Public Radio about the people of Fort Scott and how their health care transformed after the hospital closed. “Where It Hurts” is available wherever you get your podcasts.
