- Social Factors Help Explain Worse Cardiovascular Health among Adults in Rural Vs. Urban Communities
- Reducing Barriers to Participation in Population-Based Total Cost of Care (PB-TCOC) Models and Supporting Primary and Specialty Care Transformation: Request for Input
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- Secretary Kennedy Renews Public Health Emergency Declaration to Address National Opioid Crisis
- 2025 Marketplace Integrity and Affordability Proposed Rule
- Rural America Faces Growing Shortage of Eye Surgeons
- NRHA Continues Partnership to Advance Rural Oral Health
- Comments Requested on Mobile Crisis Team Services: An Implementation Toolkit Draft
- Q&A: What Are the Challenges and Opportunities of Small-Town Philanthropy?
- HRSA Administrator Carole Johnson, Joined by Co-Chair of the Congressional Black Maternal Health Caucus Congresswoman Lauren Underwood, Announces New Funding, Policy Action, and Report to Mark Landmark Year of HRSA's Enhancing Maternal Health Initiative
- Biden-Harris Administration Announces $60 Million Investment for Adding Early Morning, Night, and Weekend Hours at Community Health Centers
- Volunteer Opportunity for HUD's Office of Housing Counseling Tribe and TDHE Certification Exam
- Who Needs Dry January More: Rural or Urban Drinkers?
- Rural Families Have 'Critical' Need for More Hospice, Respite Care
- States Help Child Care Centers Expand in Bid To Create More Slots, Lower Prices
Cost-Effectiveness of the Ryan White HIV/AIDS Program
This month, HRSA published a pair of manuscripts demonstrating the cost-effectiveness of the Ryan White HIV/AIDS Program (RWHAP) in the Journal of Acquired Immune Deficiency Syndromes (JAIDS).
These two papers present findings from the first formal evaluation of the RWHAP’s cost-effectiveness at a national level. The first paper presents a new and innovative mathematical model that can be used as a tool for estimating the cost-effectiveness of the RWHAP under a variety of policy scenarios and assumptions. The second paper compares estimated health care costs and outcomes over a 50-year period in the presence of the RWHAP relative to those expected if the comprehensive and integrated system of medical and support services funded by the RWHAP were not available.
Read the first paper.
Read the second paper.
Rural Health System Part of Operation Warp Speed Trials for Covid-19 Treatments

By Liz Carey
On the Canadian border of Upstate New York, a small health system is a rare example of rural-based clinical trials for treating Covid-19.
Read more
Report: To Fix Rural Problems We Have to Overhaul Existing Rural Programs

By Anya Slepyan
Researchers found that the federal development programs aimed at partnering with rural communities are ineffective in the rural environment of today.
Read more
White House Staffers Brief Rural Health Advocates on Biden’s American Rescue Plan

By Liz Carey
The Biden administration wants to provide vaccines to federally qualified health centers serving hard-to-reach populations. Also on the table is $160 billion in community support for supplies, testing, and public health personnel.
Read more
Rural Transit Systems Must Balance the Safety of Passengers and Drivers

By Olivia Weeks
The pandemic challenged rural transit systems with maintaining their services and keeping everyone on board safe.
Read more
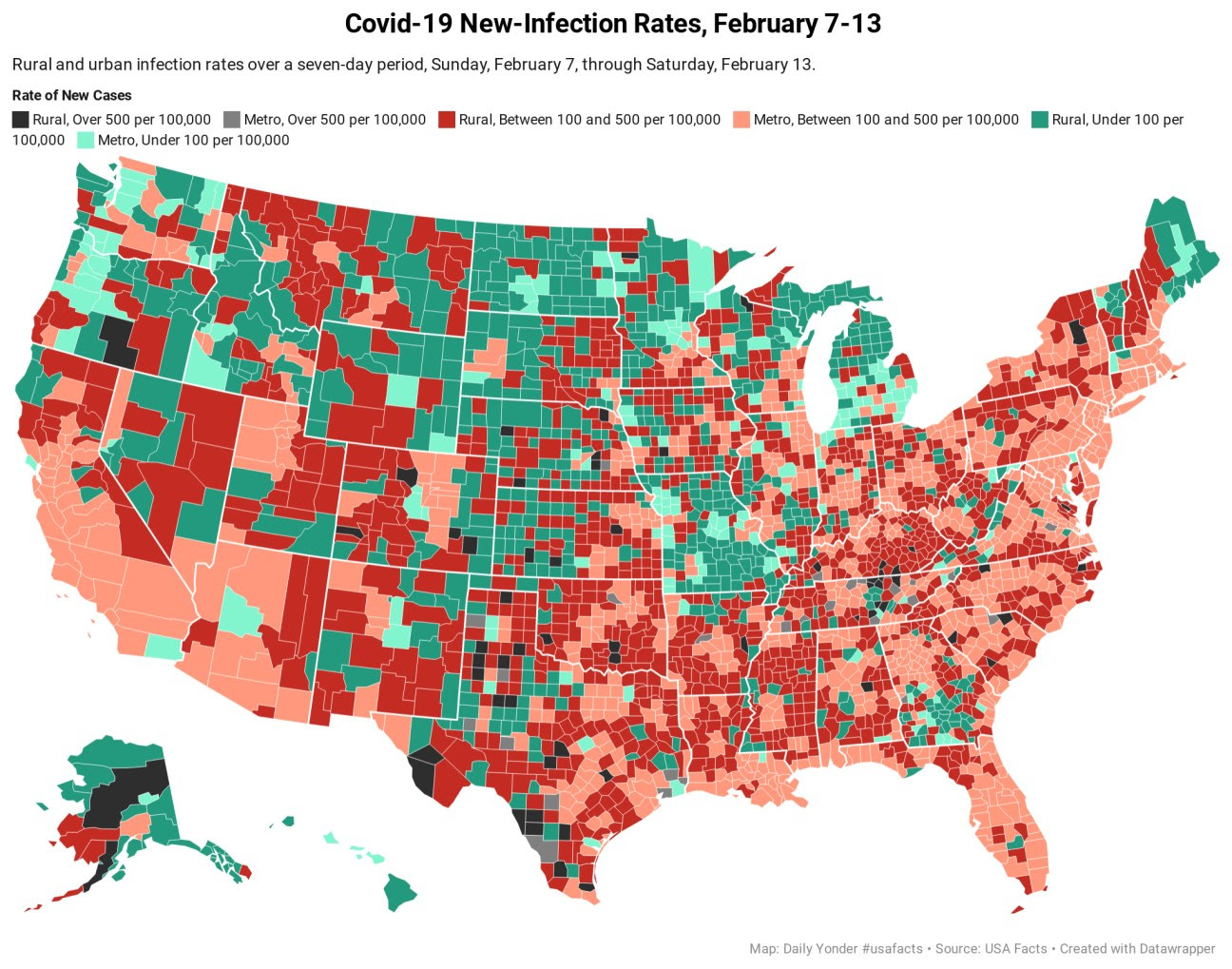
Rural Covid-19 Cases Drop While Rural Death Rate Holds Steady

By Tim Murphy and Tim Marema
The impact of the winter surge continues to be felt in the number of Covid-related deaths that occurred in rural America last week.
Read more
Expanding Diabetes Prevention and Management through Health Center Outreach
According to the Community Preventive Services Task Force, Community Health Workers (CHWs) may address a broad range of health issues and include interventions that focus on diabetes among members of their community. Interventions are delivered to community groups or individuals at increased risk of type 2 diabetes, primarily through information on improvements in diet, physical activity, and weight. This training, hosted by the National Center for Health in Public Housing, will address diabetes resources for CHWs, explain the roles and competencies of CHWs in diabetes prevention and how CHWs can help patients with diabetes with food insecurity and other social determinants of health via community resources. Learn more and register.
Quarterly Heart Health Office Hours and Other Resources
The Health Resources and Services Administration (HRSA) is celebrating American Heart Month this year by launching a quarterly Heart Health Office Hours. It is a web-based learning series highlighting evidence-based interventions to improve heart health. The inaugural session–Are Hypertension Control Innovations that Maximize Team-Based Care Effective?–on Thursday, Feb. 25 at 3:00 pm, will feature two health centers sharing their experiences implementing team-based care to improve hypertension control. Registration is required. You can also access a suite of resources from NIH’s National Heart, Lung, and Blood Institute, hypertension toolkits from the CDC, and The Surgeon General’s Call to Action to Control Hypertension that outlines goals and strategies to improve hypertension control. The National Association of Community Health Centers (NACHC) has also provided the following resources: Roadmap Quality Improvement Tool to Improve Blood Pressure Control for African Americans, NACHC SMBP Implementation Toolkit, Million Hearts® national SMBP Forum, and their Hypertension Screening and Control Action Guide.
Telehealth “Passport” Cuts through Licensing Red Tape
The Federation of State Medical Boards has launched Provider Bridge, a license-portability initiative that will allow certain clinicians to work across state lines. Clinicians can register and receive a digital Provider Bridge Passport, which collects their active licenses, disciplinary history, specialty certifications and DEA registration and NPI numbers. The clinicians can then submit that passport to a health system, hospital or other care provider in need of help. It’s currently limited to physicians and physician assistants, but the Federation plans to expand the program to other healthcare professionals. Read more.
Biden Extends Forbearance on Student Loans
On his first day in office, President Biden fulfilled his promise to extend forbearance on federal student loans. That means those with Federal student loans do not need to make payments until October 2021. Interest on these loans remains at zero percent during this time. This applies to:
- All Direct Loans (including those in default)
- All FFEL Program loans (including those in default)
- All Federal Perkins Loans (including those in default)
- Defaulted HEAL loans
President Biden has also indicated that he wants to reform and expand certain elements of federal loans, including parts of Public Service Loan Forgiveness, but those actions will come later.
